Verification of Benefits with Reveloop
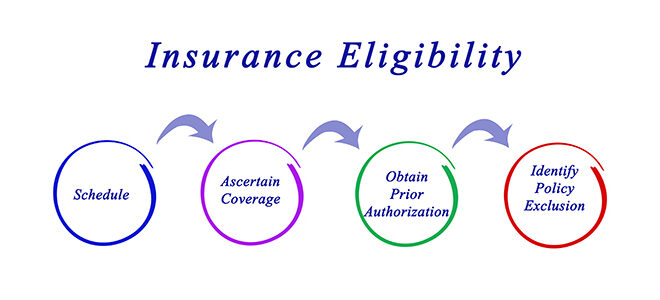
Reveloop introduces advanced eligibility and benefits verification services for behavioral healthcare providers, facilitating the meticulous confirmation of insurance coverage and eligibility for their patients. This strategic process serves to mitigate the risk of denied claims, culminating in an elevation of the overall revenue stream.
Contact Us Now